CHAPTER 3: Senses and Perception
In this Chapter
Touch and Pain
1Touch is the sense by which we determine the characteristics of objects: size, shape, and texture. We do this through touch receptors in the skin. In hairy skin areas, some receptors consist of webs of sensory nerve cell endings wrapped around the base of hairs. The nerve endings are remarkably sensitive. They can be triggered by the slightest movement of the hairs.
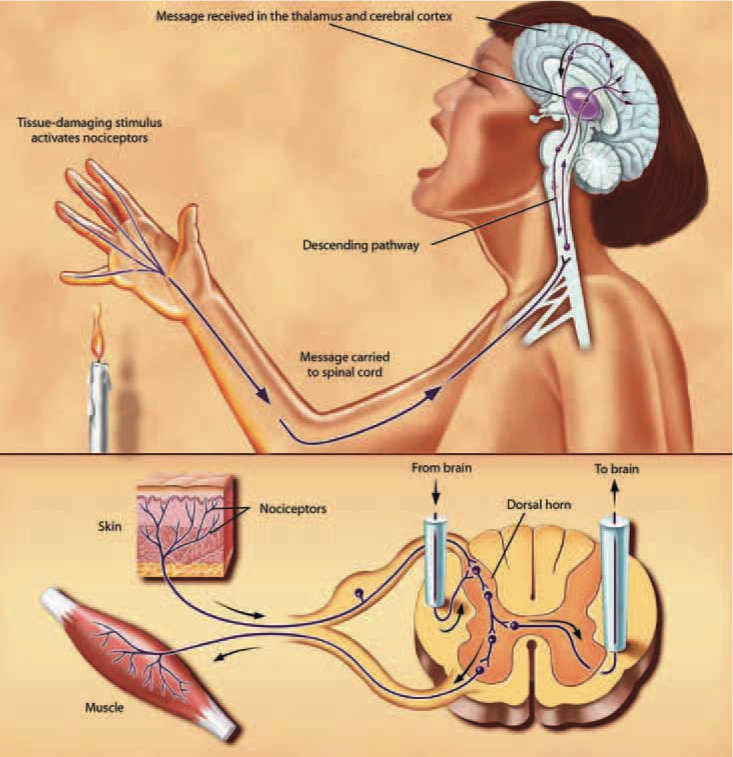
2Signals from touch receptors pass via sensory nerves to the spinal cord, where they synapse, or make contact with, other nerve cells, which in turn send the information to the thalamus and sensory cortex. The transmission of this information is highly topographic, meaning that the body is represented in an orderly fashion at different levels of the nervous system. Larger areas of the cortex are devoted to sensations from the hands and lips; much smaller cortical regions represent less sensitive parts of the body.
3Different parts of the body vary in their sensitivity to tactile and painful stimuli. These varying responses are based largely on the number and distribution of receptors. For example, the cornea is several hundred times more sensitive to painful stimuli than are the soles of the feet. The fingertips are good at touch discrimination, but the torso is not.
4Neurologists measure sensitivity by determining the patient’s two-point threshold, the distance between two points on the skin necessary in order for the individual to distinguish two distinct stimuli from just one. This method involves touching the skin with calipers at two points. Not surprisingly, acuity is greatest in the most densely nerve-packed areas of the body. The threshold is lowest on the fingers and lips.
5The sensory fibers that respond to stimuli that damage tissue and can cause pain are called nociceptors. Different nociceptor subsets produce molecules that are responsible for the response to noxious (i.e., painful) thermal, mechanical, or chemical stimulation. Interestingly, these same molecules respond to plant-derived chemicals, such as capsaicin, garlic, and wasabi, that can produce pain. Some nociceptors in the skin respond to chemical stimuli that cause itch. Histamine is an example of such a nociceptor, and it can be released in response to certain bug bites or allergies.
6Tissue injury also causes the release of numerous chemicals at the site of damage and inflammation. Prostaglandins enhance the sensitivity of receptors to tissue damage and ultimately can induce more intense pain sensations. Prostaglandins also contribute to the clinical condition of allodynia, in which innocuous stimuli can produce pain, as when sunburned skin is touched.
7Persistent injury can lead to changes in the nervous system that amplify and prolong the "pain" signal. The result is a state of hypersensitivity in which pain persists and can even be evoked by normally innocuous stimuli. Persistent pain is in many respects a disease of the nervous system, not merely a symptom of some other disease process.
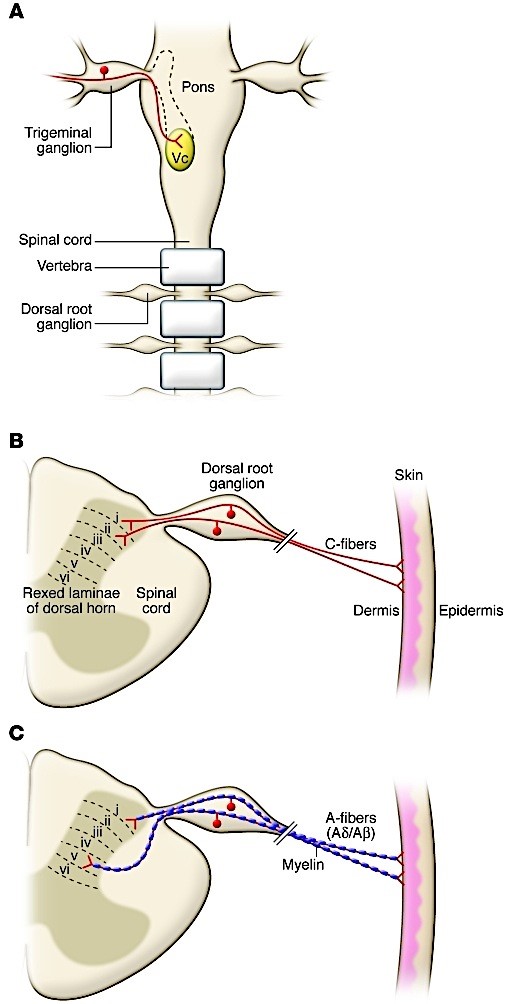
8Sending and Receiving Pain and Itch Messages. Pain and itch messages are transmitted to the spinal cord via small, myelinated fibers and C fibers, very small, unmyelinated fibers. The myelinated nerve fibers are very pain-sensitive, and they probably evoke the sharp, fast pain that is produced by, for example, a pinprick. C fiber-induced pain, by contrast, is generally slower in onset, dull, and more diffuse.
9In the ascending system, impulses are relayed from the spinal cord to several brain structures, including the thalamus and cerebral cortex. These structures are involved in the process by which pain or itch messages become a conscious experience. The experience of pain or itch is not just a function of the magnitude of the injury or even the intensity of the impulse activity generated. Other factors, such as the setting in which the injury occurs (e.g., in childbirth or in a car accident), as well as the emotional impact, also determine our overall response to the experience.
10Pain messages can be suppressed by systems of neurons that originate within the gray matter in the brainstem. These descending systems suppress the transmission of pain signals from the dorsal horn of the spinal cord to higher brain centers. Some of these descending systems use naturally occurring chemicals, the endogenous opioids, or endorphins, which are functionally similar to morphine. Recent findings indicating that endorphins act at multiple opioid receptors in the brain and spinal cord have had important implications for pain therapy. For example, scientists began studying how to deliver opioids into the spine after discovering a dense distribution of opioid receptors in the spinal cord horn. After a technique for delivering opioids into the spine was used successfully in animals, such treatments were begun in humans; the technique is now common in treating pain after surgery.
11 Modern imaging tools are used to help scientists better understand what happens in the brain when pain is experienced. One finding is that no single area in the brain generates pain; rather, emotional and sensory components together constitute a mosaic of activity leading to pain. Interestingly, when people are hypnotized so that a painful stimulus is not experienced as unpleasant, activity in only some areas of the brain is suppressed, showing that the stimulus is still experienced. It just doesn’t hurt anymore. As such techniques for brain study improve, it should be possible to monitor the changes in the brain that occur in people with persistent pain more effectively and to better evaluate the different painkilling drugs being developed.
13Processing information from the sensory systems is only one of many functions of the brain. Such information is often the first step in other brain activities, including learning and retaining knowledge. The next chapter discusses what we know about these key functions as well as where gaps in our understanding remain.