Chapter 14: Injury and Illness
In this Chapter
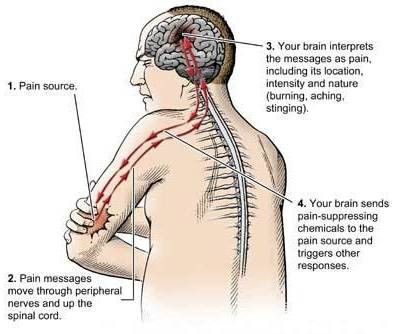
Pain
1If there is a universal experience, it is pain. Each year, more than 76.2 million Americans suffer chronic, debilitating headaches or a bout with a bad back or the pain of arthritis — all at a total cost of some $100 billion. But it need not be that way. New discoveries about how chemicals in the body transmit and regulate pain messages have paved the way for new treatments for both chronic and acute pain.
2 Treating Pain Local anesthesia, or loss of sensation in a limited area of a person’s body, is used to prevent pain during diagnostic procedures, labor, and surgical operations. Local anesthetics temporarily interrupt the action of all nerve fibers, including pain-carrying ones, by interfering with the actions of sodium channels. Historically, the most familiar of these agents was Novocain, which has been used by dentists for years. Lidocaine is more popular today.

3Analgesia refers to the loss of pain sensation. The four main types of analgesics, or painkillers, are nonopioids, which refer to aspirin and related nonsteroidal anti-inflammatory drugs, or NSAIDs. Common NSAIDs include ibuprofen and naproxen. Opioids (morphine, codeine), antiepileptic agents (gabapentin, topiramate), and antidepressants (amitriptyline, duloxetine) are the other three types of analgesics. Acetaminophen, the active ingredient in Tylenol, has analgesic properties but does not reduce inflammation.
4NSAIDs are useful for treating mild or moderate pain, such as headache, sprains, or toothache. Because NSAIDs are anti-inflammatory, they also are effective for treating injuries or conditions such as arthritis and postoperative pain. NSAIDs work by inhibiting the cyclo-oxygenase (COX) enzymes that make the inflammatory and painproducing chemical prostaglandin. Often moderate pain is treated by combining a mild opioid, such as codeine, with aspirin or an NSAID. Opioids are the most potent painkillers and are used for severe pain. Opioids, however, have many adverse side effects, such as respiratory depression and constipation, and in some individuals they have a high potential for abuse.
5Antiepileptic and antidepressant drugs are useful primarily for neuropathic pain, which comes from injury to the nervous system. Such pain includes the pain from diabetic neuropathy, or damage to nerves in the body resulting from high blood sugar levels; neuralgia, or nerve pain or numbness, from viruses such as shingles; phantom limb pain; and post-stroke pain. The best results have been reported with antidepressants that regulate both serotonin and norepinephrine. Interestingly, SSRIs, which selectively affect serotonin, do not help relieve neuropathic pain. For some neuropathic pain conditions in which a light touch to the skin can produce severe pain, topical lidocaine may be effective.
6 The Body’s Pain-Control System Studies of the body’s own pain-control system not only demonstrated the existence of naturally occurring opioids — the endorphins — but also identified the receptors through which opioids exert their effects. The finding that opioid receptors are concentrated in the spinal cord led to the use of injections of morphine and other opioids into the cerebrospinal fluid in which the spinal cord is bathed, without causing paralysis, numbness, or other severe side effects. This technique came about through experiments with animals that first showed that injecting morphine into the spinal fluid could produce profound pain control. It is now commonly used in humans to treat pain after surgery, and to treat chronic pain in some patients by having them use an implanted pump.
7New targets are on the horizon. Molecular biology and genetic approaches have identified many molecules, such as ion channels and receptors, which are predominantly, if not exclusively, expressed by the nociceptor, the peripheral nerve fiber that initially responds to the injury stimulus. Because adverse side effects of drugs arise from the widespread location of the molecules targeted by analgesics — for example, constipation results from morphine’s action on opioid receptors in the gut — new analgesics that target only the nociceptor may have fewer side effects. Among the many nociceptor targets are specialized receptor channels — one of which is activated by capsaicin, the pungent ingredient in hot peppers, and another by mustard oil — as well as a variety of acid-sensing sodium and calcium ion channels. Blocking the activity of many of these molecules has proven effective in animal studies, suggesting that the development of drugs that target these molecules in humans may have great value for the treatment of acute and persistent pain. Following from these findings, topical (skin) application of high doses of capsaicin has recently been approved for some neuropathic pain conditions. This treatment likely kills the sensing portion of pain fibers, but because these nerve fibers will regenerate, treatment needs to be repeated.
8Pain is a complex experience that is largely a product of brain function. The pain is in the brain, not in the nociceptors that respond to the injury. Pain also involves emotional factors, so previous experiences with pain can have an impact on a more recent experience. All of these variables must be addressed concurrently in order to treat pain. The fact that placebos and hypnosis can significantly reduce pain clearly illustrates the importance of these psychological factors.
